Understanding pulmonary fibrosis
Pulmonary fibrosis, also known as lung fibrosis or lung scarring, is a rare condition that can affect a person’s ability to breathe.1

Disease progression
Many types of pulmonary fibrosis (PF) are progressive conditions, such as idiopathic pulmonary fibrosis (IPF) and progressive pulmonary fibrosis (PPF). This means the lung tissue will become thicker and more scarred over time. It’s important to understand that progression is about the disease itself, not just the symptoms you may feel.2-5
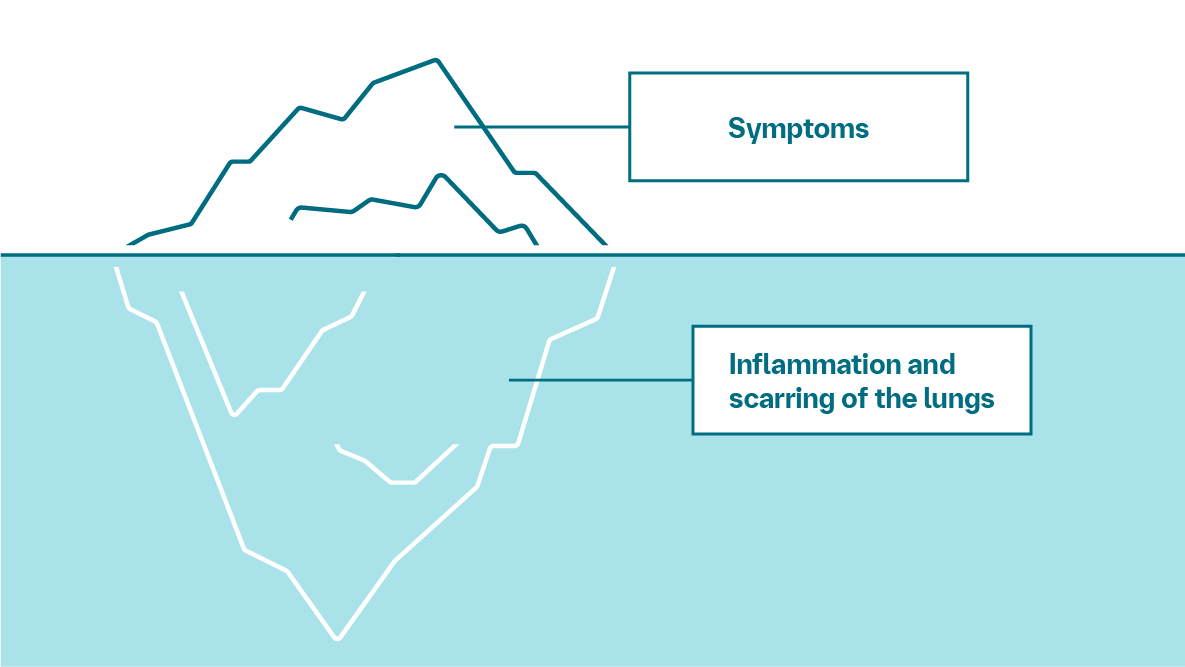
Think of PF as an iceberg
On the surface, there are symptoms that may be hard to ignore. But below the surface, IPF and PPF cause something even more serious— inflammation and scarring of the lungs that get worse over time.2,3,6-8
As IPF and PPF progress, symptoms get worse and lungs don’t function as well as they should—and this damage cannot be undone.3
What are the signs of disease progression?

Your doctor can perform tests to measure this, such as forced vital capacity (FVC)9,10

This may include shortness of breath, cough, or fatigue3

Your doctor can see scarring with a high-resolution CT scan10
How does disease progression affect me?
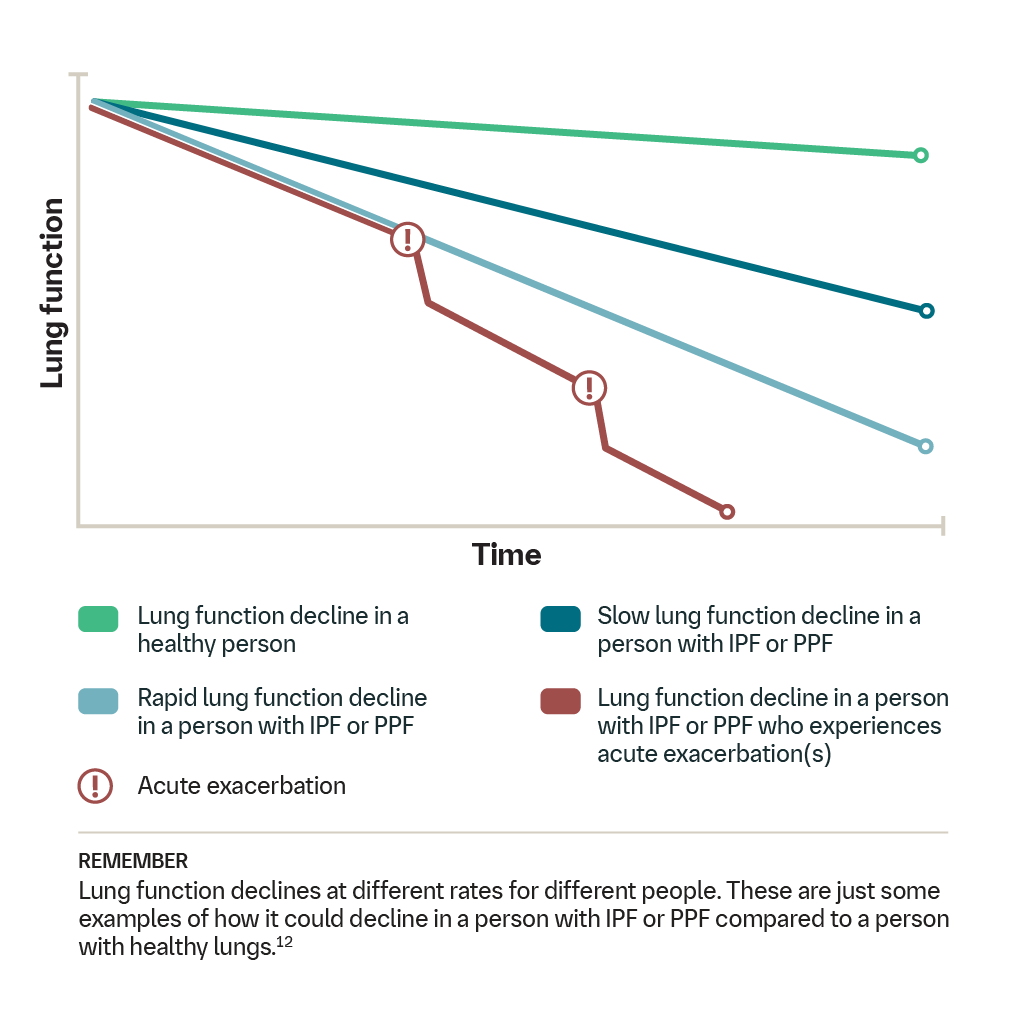
The progression of PF will cause your lung function to decline. Looking at this graph, you can see that, in a person with healthy lungs, lung function gradually declines as the person gets older.3
In a person who has IPF or PPF, disease progression causes lung function decline to happen more quickly, which makes breathing more difficult. Additionally, some people living with IPF or PPF may experience an acute exacerbation—a sudden decline in lung function along with worsening lung scarring.3,5,7,11
As PF gets worse, it can also:

Progression will make breathing challenging and, as a result, you may feel more tired and have trouble moving around. This can make it harder to reach daily and long-term goals, like working, exercising, traveling, or spending time with your loved ones.3,5,7

Your voice matters when choosing your treatment plan
Talking to your care team about your treatment goals can help inform critical decisions about the best options. It’s important to know how well certain options may work and how they may affect your body.
In conversations with your care team, you should also ask questions, raise concerns, and speak honestly about how treatment will fit into all aspects of your life—physically, mentally, or financially.
Setting goals and following a care plan can help you feel more in control of PF.
Talk to your doctor about treatment options. A good treatment plan may help you slow the progression of PF. There are many different treatment options.10
Abbreviations: CT, computed tomography; FVC, forced vital capacity; IPF, idiopathic pulmonary fibrosis; PF, pulmonary fibrosis; PPF, progressive pulmonary fibrosis.
-
Meltzer EB, Noble PW. Idiopathic pulmonary fibrosis. Orphanet J Rare Dis. 2008;3:8.
-
Cottin V. Criteria for progressive pulmonary fibrosis: getting the horse ready for the cart. Am J Respir Crit Care Med. 2023;207(1):11-13.
-
Mayo Clinic Staff. Pulmonary fibrosis. Updated February 15, 2024. Accessed September 2, 2025. https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis
-
American Lung Association. Pulmonary fibrosis progression and exacerbation. Updated June 7, 2024. Accessed September 2, 2025. https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-fibrosis/patients/living-well/progression-and-exacerbation
-
Cleveland Clinic. Pulmonary fibrosis. Last reviewed April 5, 2021. Accessed September 2, 2025. https://my.clevelandclinic.org/health/diseases/21431-pulmonary-fibrosis
-
Rajan SK, Cottin V, Dhar R, et al. Progressive pulmonary fibrosis: an expert group consensus statement. Eur Respir J. 2023;61(3):2103187.
-
Asthma + Lung UK. What is pulmonary fibrosis? Updated June 1, 2022. Accessed September 2, 2025. https://www.asthmaandlung.org.uk/conditions/pulmonary-fibrosis/what-pulmonary-fibrosis
-
National Heart, Lung, and Blood Institute. What is idiopathic pulmonary fibrosis? National Institutes of Health. Updated June 26, 2023. Accessed September 2, 2025. https://www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis
-
Cleveland Clinic. Lung diffusion testing (DLCO). Last reviewed February 8, 2024. Accessed September 2, 2025. https://my.clevelandclinic.org/health/diagnostics/15445-lung-diffusion-testing-dlco
-
Mayo Clinic Staff. Pulmonary fibrosis: diagnosis and treatment. Updated February 15, 2024. Accessed September 2, 2025. https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis/diagnosis-treatment
-
Wong AW, Ryerson CJ, Guler SA. Progression of fibrosing interstitial lung disease. Respir Res. 2020;21(1):32.
-
Podolanczuk AJ, Thomson CC, Remy-Jardin M, et al. Idiopathic pulmonary fibrosis: state of the art for 2023. Eur Respir J. 2023;61(4):2200957.
-
Lung Foundation Australia. Managing progression in pulmonary fibrosis. Published February 2024. Accessed September 2, 2025. https://lungfoundation.com.au
-
American Lung Association. Coping with stress and emotions from pulmonary fibrosis. Updated June 7, 2024. Accessed September 2, 2025. https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-fibrosis/patients/living-well/coping-with-stress